A Leading Expert
in Joint Resurfacing, Cartilage Restoration, Shoulder & Knee Conditions.
Keeping You GOING Strong At Every Stage Of Life
Salt Lake City & Park City, UT
-Currently Accepting New Patients-
- Dr. Phil Davidson is a renowned Orthopedic Physician practicing in Salt Lake City and Park City, Utah. He is sought after for his cutting edge surgical techniques, to especially include cartilage restoration and joint resurfacing of the knee and shoulder. He specializes in the treatment of sports injuries and “wear and tear” joint issues.
- Many patients come to see Dr. Davidson to explore alternatives to total knee and shoulder replacement. Treatment is customized to each patient with an ever-expanding array of individualized options that may avoid or delay a total joint replacement. Dr. Davidson does perform state-of-the-art total knee and shoulder replacements when necessary.
- Dr. Davidson provides personalized dedicated care with a commitment to comprehensive surgical and non-surgical treatment plans.
Click the link to listen.
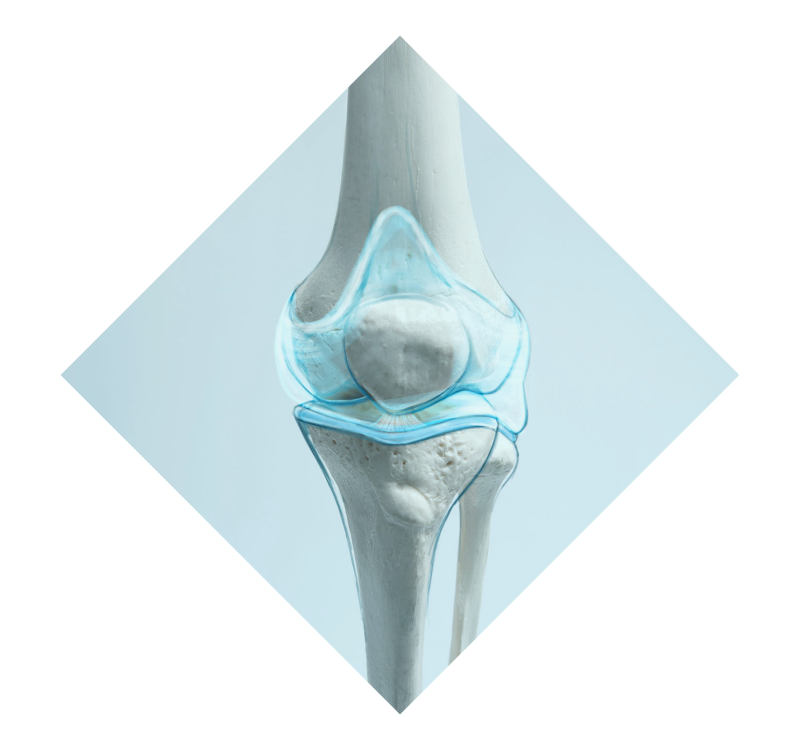
JOINT RESURFACING
Joint Resurfacing is a surgical approach that restores only the damaged part of the joint, preserving all the healthy components. This is more minimally invasive than Total Joint Replacement.
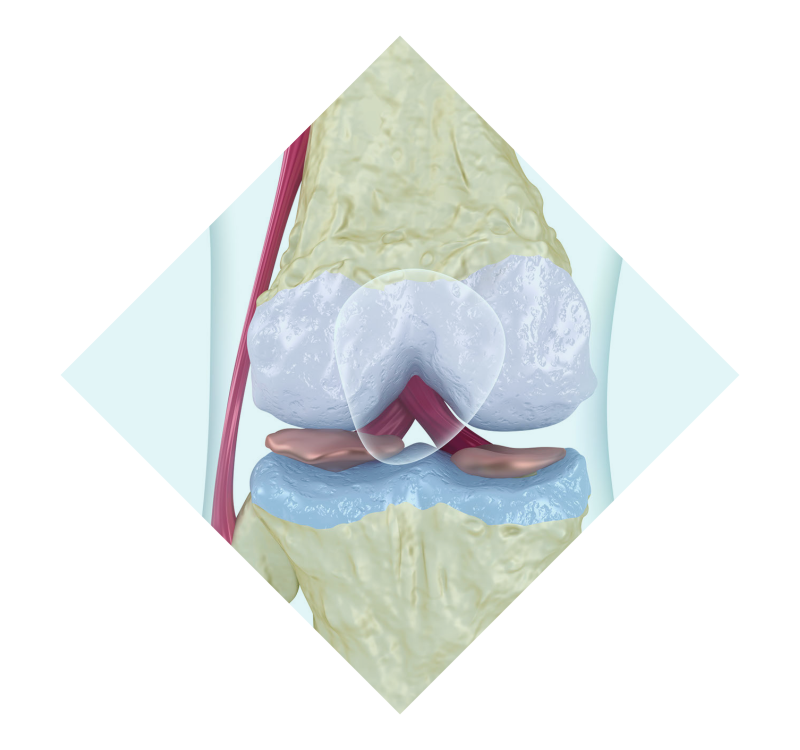
cartilage restoration
Cartilage Restoration is an array of treatments and procedures designed to restore the natural lining and tissues of the joint.
sports injuries
Sports Injury treatment is a variety of procedures to repair and restore damaged knee and shoulder tissues. Including Knee: ACL tears, Meniscus Tears, Patellofemoral (knee cap) Pain. Shoulder: Rotator Cuff Tears, Shoulder instability and labral tears.
KNEE SURGICAL PROCEDURES
Dr. Davidson has made it the guiding principle of his practice to offer an ever increasing array of surgical options to restore damaged knees and help return patients to active lifestyles.
SHOULDER SURGICAL PROCEDURES
Dr. Davidson uses the most current techniques to repair, reconstruct and resurface damaged shoulders as needed. Patients come to Dr. Davidson for treatment of a wide variety of shoulder concerns.

Surgical and Non-Surgical
Dr. Davidson provides personalized dedicated care with a commitment to comprehensive surgical and non-surgical treatment plans.
Pick Up Right Where You Left Off!
Meet Dr. Davidson! Get An Accurate Diagnosis & Comprehensive Treatment Plan.
a long list of Success Stories

COVID 19: Update:
During the COVID-19 Outbreak we are here for you at Davidson Orthopedics.
– Our entire team has been vaccinated & we continue to practice in accordance with CDC Guidelines.
– At Davidson Orthopedics, we care about our patient’s safety and access to healthcare.
– We are offering both in-person & virtual consultations and appointments.
Send Us A Message!
Take The First Step!
435-608-9900